Improving healthcare for Black African and Caribbean communities
A team from the NHS Black Country Integrated Care Board (ICB) has been leading on a unique project to help improve healthcare for Black African and Caribbean communities in the Black Country.
Using funding from the West Midlands Cancer Alliance, the Involvement Team has worked with partners from across the Black Country to understand the barriers Black African and Caribbean women face when attending breast screening appointments and raise awareness of the signs and symptoms of breast cancer.
As part of the project, eight local voluntary and community sector organisations were commissioned to host conversations with local women in the community to help identify first-hand the barriers and stigmas in attending screening appointments or presenting at GPs with early symptoms.
The insight gathered from these groups was used to co-design solutions and interventions over a course of three workshops, led by Dr Martin Bollard, Head of Nursing in the Faculty of Health and Wellbeing at the University of Wolverhampton.
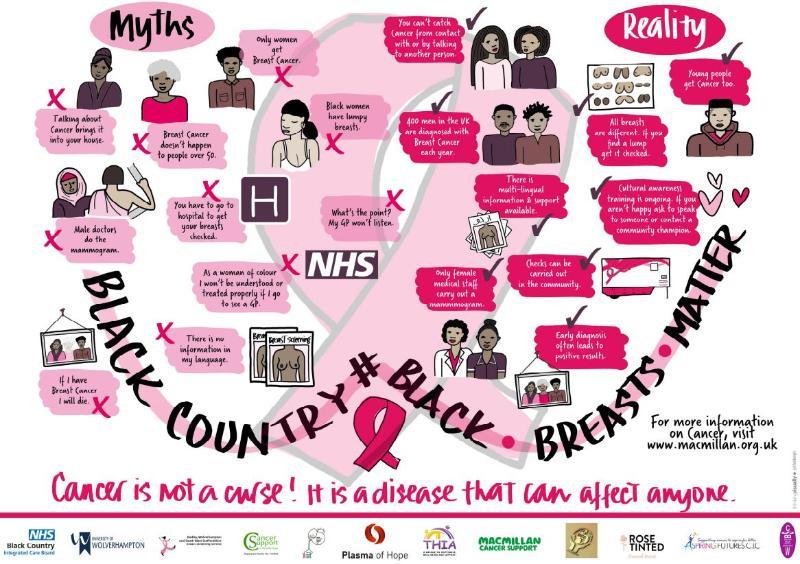
This includes an infographic which tells their stories, which can be found on the Black Country ICB website here, and a video of a local mother and daughter having a myth busting conversation, which can be viewed on YouTube here.
Marie-Claire Kofi is Chief Executive Officer of Plasma of Hope, a charity that provides supports for people living with sickle cell disease across the West Midlands and is one of the organisations that took part in the project.
She said: “When I heard about the project, I knew immediately that I wanted to be involved as it’s an important topic that has a huge impact on our community and we simply don’t talk about it enough. We hosted a number of sessions with the women and families that our organisation supports to discuss breast cancer, and we got a lot of different perspectives. Some assumed that only people over a certain age get breast cancer, and many didn’t know how to properly check their breasts.
“A key theme we spotted was that families didn’t want to talk about cancer, as they believed talking about it meant you were more likely to get it as you are welcoming it in. As a black woman, I can resonate with this, as I was also brought up not to talk about certain things. Because of the culture we come from, where topics like health issues aren’t discussed, there’s a real lack of awareness within the black community.
“Not talking about breast cancer doesn’t make the problem go away, so it was great to have these important conversations and help people understand and recognise the changes and what to look out for and dispel some of the myths around breast cancer.”
Althea Wint is the founder and director of THIA, a not-for-profit organisation supporting the wellbeing of children and their families in the Black Country and Birmingham that also took part in the project. She said: “We held a number of interactive workshops in the community which took place over a week. The turnout was fantastic – we had more than 50 women attend, as well as men too who wanted to find out how they could support their partners, family members and friends when it comes to breast cancer.
“The biggest barriers that we found from the women we spoke to were around feeling ashamed of their bodies, not knowing how to examine themselves, the fear of not knowing where to go or what was next and a fear of not being taken seriously by their doctor. This project is something that is also very personal to me. I had a breast cancer scare and I have had close friends and family affected by breast cancer.
“I think representation is really important as well when it comes to making people feel comfortable and engaged. Something that worked really well at our sessions was having an example of a black breast to demonstrate how to check your breasts for lumps. It might seem small and unimportant, but being able to show women a breast they could relate to and identify with, rather than a white one, made such a difference. I have been working with the screening team to identify a diverse black breast cancer model for future sessions.”
A number of the organisations who hosted the sessions have since taken part in Cancer Champion training. Hosted by the NHS Black Country ICB, the training program is designed in partnership with Cancer Research UK and gives participants the knowledge and confidence to have conversations in their community about cancer prevention, the importance of screening and early diagnosis.
Dr Martin Bollard, Head of Nursing in the Faculty of Education, Health and Wellbeing at the University of Wolverhampton, has been leading the project and said: “I am delighted to have had the opportunity to work alongside the Black Country ICB and the wonderful, female, black African and Caribbean community leaders, representing hundreds of women across the Black Country. In a short space of time, we have captured the narrative on breast cancer screening from hundreds of women and shaped that ‘lived experience’ into products to share with others.
“This is helping to demystify some of the cultural taboos on breast cancer and raise awareness of the importance of early breast cancer diagnosis for this group of women. It’s been an absolute privilege being part of this project and I look forward to mobilising more knowledge on this important topic over the months ahead.”
Three of the organisations who have been involved in the project will be also attending the Black Women and Breast Cancer 5th Annual Conference, which takes place in London on Saturday 21 October, to raise awareness of the Black Breasts Matter project and the insights that have been gathered in the Black Country.
Diane Wake, Cancer Lead for the Black Country Integrated Care System, said: “This is an important piece of work which has helped identify some of the barriers that Black African and Caribbean women face when attending breast screening and GP appointments in the Black Country.
“We know lives are saved when cancers are caught early, and I would urge anyone who has received a breast screening invitation – even if you received the invite weeks or months ago – to make an appointment – it could save your life.
“This month is also Breast Cancer Awareness Month, so I’d like to take this opportunity to remind women of all ages of the importance of being breast aware. This means getting to know how your breasts look and feel at different times, so you know what’s normal for you and telling your doctor straight away if you notice any unusual changes.”
Under the NHS Breast Screening Programme eligible women will receive their invite for breast cancer screening every three years between the ages of 50 and 71. Women should look out for their invite letter and follow the instructions to book an appointment.
If you think you’ve missed your breast screening appointment, or you have not been invited by the time you are 53, you should contact your local breast screening service. You can find your local breast screening service on the NHS website here.
For more information on breast screening, please visit the NHS Black Country ICB website here.
ENDS
Notes to editors
- The eight VCSE organisations that took part in the project included Aspiring Futures, Bread4Life, Migrant Empowerment Group, Plasma of Hope, Rose Tinted Financial Services, THIA, Walsall Black Sisters Collective and Whitehouse Cancer Support.
- For media enquiries email comms.blackcountry@nhs.net
- The Black Country Integrated Care System (ICS) was formed on 1 July 2022, following passage of the Health and Care Act 2022.
- Our ICS, known as Healthier Futures, brings providers and commissioners of NHS services together with local authorities and other local partners to plan and deliver joined up services and to improve the lives of people who live and work in the Black Country.
- Black Country ICS includes the Integrated Care Board (ICB), Integrated Care Partnership (ICP), place-based partnerships and provider collaboratives.
- Together, these partners serve a local population of 1.26 million people living in the second most deprived ICS in England.
- For more information about the ICS, our purpose and priorities, visit our website or follow us on social media:
- Website: www.blackcountryics.org.uk
- Twitter: @BlackCountryICS
- Facebook: @BlackCountryICS
For more information please contact the Corporate Communications Team.


/prod01/wlvacuk/media/departments/digital-content-and-communications/images-2024/240624-Alumni-Awards-2024-Resized.jpg)
/prod01/wlvacuk/media/departments/digital-content-and-communications/images-18-19/220325-Engineers_teach_thumbail.jpg)
/prod01/wlvacuk/media/departments/digital-content-and-communications/images-2024/240627-UN-Speaker-Resized.jpg)
/prod01/wlvacuk/media/departments/digital-content-and-communications/images-2024/240320-Uzbekistan-Resized.jpg)
/prod01/wlvacuk/media/departments/digital-content-and-communications/images-2024/240229-The-Link-Resized.jpg)
/prod01/wlvacuk/media/departments/digital-content-and-communications/images-2024/240627-Lady-Aruna-Building-Naming-Resized.jpg)